Abstract
Background Stroke in cancer patients is common due to multiple mechanisms including direct tumor related, coagulation disorders, infections and therapy related. There have been few studies associating risk of stroke with different types of cancers including non-Hodgkin's lymphoma (NHL). However, literature on association of mortality in patients with stroke and non-Hodgkin's lymphoma is sparce. Aim of our study was to examine the morbidity and mortality in NHL patients admitted with acute ischemic stroke.
Methodology All adult hospitalized patients from January 2016 to December 2019 in the nationwide inpatient sample were captured. The study population included all patients with a primary diagnosis of Acute Ischemic stroke. The population was divided into patients with underlying NHL (Study) and those without it (Control). We used Wilcoxon rank sum test for comparing continuous variables and Chi-square tests for categorical variables. For univariate and multivariate analysis, we performed univariate and multivariate logistic regression models respectively. The primary outcome was mortality rates and secondary outcomes were morbidity rates and healthcare utilization.
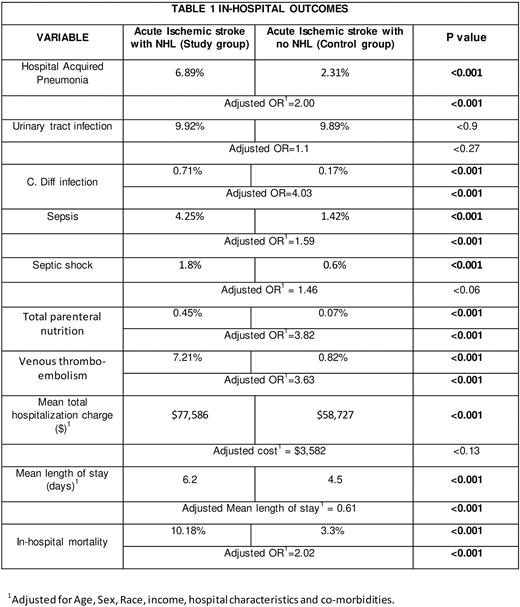
Results The sample size included 2,534,589 adult patients with acute ischemic stroke, of which 2,526,824 (99.7%) had no documented non-Hodgkin's lymphoma while 7765 (0.3%) did. The mean age of patients in both the groups was 70 years. Sex-distribution was approximately equal with no significant difference between the two groups. Patients with NHL had increased In-hospital mortality (Adjusted OR: 2.02, p<0.001). They also had increased risk of hospital acquired pneumonia (Adjusted OR (aOR): 2, p<0.001), C.diff infection (aOR: 4.03, p<0.001), Sepsis (aOR: 1.59, p<0.001), septic shock (aOR:1.46, p<0.001). The risk of developing UTIs however was insignificantly different between the two groups. Underlying NHL also increased the risk of Venous thromboembolism (aOR: 3.63, p<0.001) and requirement of Total Parental Nutrition (aOR 3.82, p<0.001) in patients admitted with acute ischemic stroke. Mean total hospitalization charge was insignificant but the mean length of stay was 0.61 days (p<0.001) higher in patients with underlying NHL.
Conclusion Patients admitted with acute ischemic stroke and underlying NHL have 2-fold higher mortality risk compared to patients without NHL. It also increases morbidity in acute ischemic stroke patients that ultimately increases the health-care utilization and burden on the patient and their families.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.